I'm on call about 10 days a month, for 24 hours at a time, usually 2 or 3 days together, then off for a few days. I'll get a call that goes something like this:"I need you to go to Springfield Medical Center(made up name, think Simpsons). The ICU called with a 24 year old male, gun shot wound to the head. He has no history. BP is 100/50. He's on multiple pressors. Urine output is 500cc an hour. Family's at the hospital. He's got a fiance, mom and dad are divorced and a big crowd of cousins, etc. 1st clinical's done. Call back when you get there and let me know what's going on."
Off I spring into action. Well, spring's a bit of a euphamism. Okay, so I haul my old bones off the couch. I have to be there within 90 minutes and the area I cover is rather large. Already packed is my bag, with laptop, organ donation literature, paperwork, calculator, pen light, snack, personal care items like toothpaste(never know how long I'll be out, could be all night)and other, assorted junk I might need. Some stuff I keep in my trunk, like memory boxes and a gauge for reading NIF's(for DCD referrals).
When I get to the unit, I introduce myself to the staff. I usually get one of two reactions:Hey! the transplant coordinator's here! or Ugh, the transplant coordinator's here. I've been called a vulture too many times to count. But I digress. I'll read through the chart and see if there's any reason this person CAN'T be a donor-HIV, cancer, multi-organ failure. There's not too many absolute rule outs anymore. Yes, we will recover organs from people with hepatitis, particularly for recipients with hepatitis. Brain tumors are okay, generally, as long as there's no metz and no VP shunt.
The reason for this, and the reason we always ask staff NOT to mention donation is this:many families want to donate....If you bring up donation and then find out that the person can't donate because of some medical condition, it's like a second heartbreak for the family. First, they have to deal with their loved one's death, but donation was a silver lining, a way to keep that person alive in someone else. So we look through the chart. If they're not medically suitable, I pack up my bag and go home.
If they can be a donor, I've got two very different jobs to do. One, talk with the hospital staff about what's going to happen next. In an ideal situation, we all "huddle"-doctors, nurses, nurse manager, chaplain, case manager, respiratory therapist-whoever's on the case and can provide insight into what needs to happen. In a bad situation, the patient's been dead on a vent for three days with docs who don't want to start brain death protocols and a family that has no idea how bad it is and keeps hoping that "he'll pull through".
The second job is to support the family. Yes, I have to keep the recipients in mind, but when you see this grieving family in front of you, you really want to do everything you can for them-out of humanity, not because "you want the organs". I try to see what the family needs-a chaplain, a room for privacy, info from the hospital. If the doctor has told them that the patient's brain dead, I'll assess them to see if they really understand. A lot of people think that brain dead means coma, that the person will be Terry Schiavo, living in a nursing home for years. But a brain dead person can't breath on their own. If the vent's shut off, they'll go into cardiac arrest. Even on the vent they'll go into multi organ failure within a few days and eventually cardiac arrest as well.
I tell people that when the brain gets injured, it swells, just like if you twist your ankle. Only the head is a closed container-a little swelling isn't too bad, but too much and the brain has no place to go, it runs out of room. Docs will try to keep this from happening with medication or sometimes surgery, even going so far as to remove a piece of the skull. Nurses keep the ICP(intercranial pressure) down by keeping stimuli to a minimum, keeping the head of the bed up at 30 degrees, etc. Sometimes this works, sometimes it doesn't. When the pressure gets too great, the only way left to go is down, through the little opening where the spinal cord, arteries and veins run. The pressure clamps down on the vessels leading to and from the brain and within minutes the brain is deprived of oxygen. Within 10 minutes, brain cells die en masse and once they're dead, that's it, there's no coming back.
Look at a nuclear brain flow and you'll see exactly what I mean. It's like the patient is wearing a black cap, except that that black space is where there is no blood flow. It's pretty dramatic.
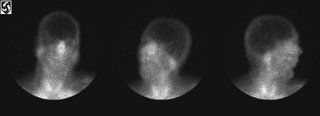
See what I mean. Maybe someday I'll write on why I hate EEG's. The picture really says it all.
At some point I'll take the family aside. I'll ask them if the patient had ever talked about his wishes, if he had a living will. I'll ask them what he or she was like. What is it like, to ask a family if they want to donate the person's organs? It ain't easy, but I think I'll have to leave that for another day.
5 comments:
challenging is not the exact word to describe your job, but i can't think of any other word.
thanks for sharing...
Yowza. You're added to my list of medblogs.
Thank you so much for sharing what you do with the rest of the blogosphere...
I'm a fascinated pharmacist, trying to get a better idea of what everybody else is doing out there, and I'm very, very pro-donation.
Keep up the good work!
I don't envy your job. It's a hard one to deal with. I am an organ and tissue donor and my family knows that I want any and all parts used by someone who can use them... I speak with people on a daily basis even though I'm not trained officially. We have to discuss living wills on admission and I usually bring up organ donation somewhere in the conversation even if it's for future reference.. Makes people think, I hope!!
I truly enjoyed reading your article. I am a soon to be nursing student who is looking into the transplant specialty. I recently went to a class regarding advocacy for patients and what it means to become a donor. As I continue to gain knowledge more pieces are fitting into this big puzzle assisting me in better understanding. Thank you for sharing!
I just interviewed for a coordinator position. Your insight into the field is incredibly helpful. During the interview they talk about how difficult it is living on call. I'm excited to see what comes out of it.
Post a Comment